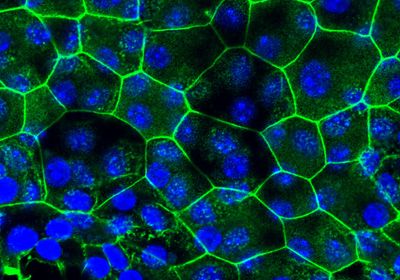
ABOVE: Differentiated bladder epithelial tissue in vitro from cells taken from mice with chronic cystitis Seongmi Russell
One of the main challenges for treating urinary tract infections is their high recurrence, especially in women. The underlying mechanisms of this high recurrence rate are not well understood, but having suffered from a previous UTI is a significant risk factor. A study in mice published April 10 in Nature Microbiology proposes that this may be partially explained because an initial urinary infection with Escherichia coli—the culprit of most UTI cases—modifies the host’s epithelial epigenome in such a way that it alters the morphology of the bladder in the long term, influencing the response to future infections by the same bacteria.
“When people think about how our body fights pathogens, they focus on the immune system,” says Shruti Naik, an immunologist at NYU Langone Health who did not participate in this study. She adds that this work shows “clear evidence that changes that occur to epithelial cells . . . have long-term consequences for how we react to” infections.
Some of the researchers behind the new study had already reported in 2016 that mice infected with an initial E. coli UTI resulted in either spontaneous resolution or a chronic cystitis, respectively reducing or increasing susceptibility to future infections. The researchers found then that, in each scenario, the E. coli UTI had differentially modified the bladder epithelium in terms of architecture, morphology, and molecular signatures. This motivated them to study the phenomenon in detail, asking, for instance, whether this remodeling occurs in “the bladder environment overall . . . or [if it is] something intrinsic to the epithelium,” says Thomas Hannan, a mucosal immunologist at Washington University in St. Louis who worked on both studies.
See “Bacteriophages Plentiful in Women’s Bladders”
For this, the team—led by Seongmi Russell, a PhD student at the time in the lab of WU’s Scott Hultgren—first isolated the epithelial stem cells from mice with either resolved or chronic infection, and cultured them to see if the cells continued to exhibit notable differences, as they had in vivo. Indeed, the fully differentiated bladder epithelium formed by these cells in vitro mimicked the morphological alterations previously observed in each group of mice. The difference between the two resulting tissues was “striking,” says Hannan. This suggested that there was “something heritable” in the cells leading to these phenotypes, he adds, “and so we hypothesized that it was an epigenetic change.”
They were right. When Hannan and his colleagues performed a series of genomic analyses on the cells, they found “different imprinting on the epigenome depending on the initial disease history, and . . . some of these could explain the phenotypes that we saw,” he says. These epigenetic alterations, namely chromatin accessibility, DNA methylation, and histone modifications, affect how several genes are expressed.
For instance, the team found that the expression of caspase-1, a gene involved in immune cell responses against microbial infections, was dramatically upregulated in the differentiated epithelium from cells of mice with chronic cystitis, while it was almost absent in those coming from mice with resolved infections as well as cells from control mice that were not exposed to E. coli. Caspase-1 induces cell death, which helps get rid of infected cells, but it also promotes inflammation and mucosal wounding, leading to an increased susceptibility to recurrent infections. Thus, the epigenetic changes observed in mice with chronic cystitis are not necessarily “all bad,” Hannan explains, “there’s a reason why we might develop” such responses—“they’re good at the time, but they may not always be good in all circumstances.”
The fact that the same changes in the bladder epithelium could be induced in vivo and in vitro suggests that the underlying epigenetic modifications “are stable and directly link to genes associated with an innate immune defense mechanism against the bacteria,” Gerard Hoyne, an immunologist at the University of Notre Dame Australia who was not involved in this work, writes in an email to The Scientist.
Translating these findings to humans—for instance, to treat recurrent UTIs—is still a distant goal, all sources agree. “A lot of other technologies would need to be in place,” says Hannan, adding that we need a “better understanding of how you can manipulate the epigenome in a very directed way” in order to develop such therapies. Hannan is Chief Scientific Officer of Fimbrion Therapeutics, a company focused on developing antimicrobial drugs to treat infectious diseases.
But the take-home message is that “when we think about infectious disease responses, we need to really start incorporating this idea that the immune system [works] in concert with the rest of the tissue,” says Naik, who had previously reported a similar inflammatory memory in the mouse skin.