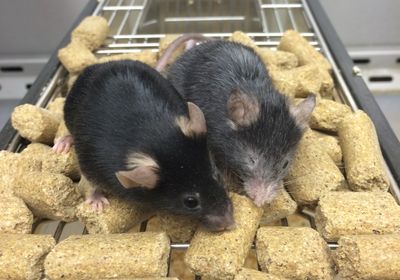
ABOVE: Ten months after a treatment that led to epigenetic disruption, mice aged much faster (R) than untreated controls (L). DAVID SINCLAIR, HARVARD MEDICAL SCHOOL
As they age, mammalian cells accrue distinct epigenetic signatures—for example, variations in DNA methylation patterns. Yet it has remained unclear whether these are a cause or a consequence of aging. A study published today (January 12) in Cell provides evidence that epigenetic disruptions alone accelerate the molecular, physiological, and neurocognitive aging in mice, and that this is driven by the cellular response to DNA damage, such as double-strand breaks (DSBs). By activating specific genes highly expressed during mammalian development, the researchers were able to restore the epigenetic landscape disrupted by the DNA repair process in their aging mouse model, leading to signs of rejuvenation.
DSBs have long been associated with aging. Because this severe form of DNA damage can lead to mutations, some researchers have hypothesized that this derived accumulation of genomic alterations could be a major cause of aging. However, in recent decades, other data have hinted that DNA damage may be involved in aging through a different pathway, one that does not involve mutations. For instance, in 2008, David Sinclair, a geneticist at the Paul F. Glenn Center for Biology of Aging Research at Harvard Medical School, and his colleagues reported that DNA breaks also lead to epigenetic disruption, in which chromatin-modifying proteins move to sites where DNA repair is needed. These rearrangements cause permanent epigenetic changes, which Sinclair and colleagues hypothesized may accumulate and promote aging in cells.
Now, in the new study, Sinclair and his colleagues tested whether this relocalization of chromatin modifiers is involved in aging. To do so, they developed a transgenic mouse model carrying a slime mold endonuclease that, when treated with the drug tamoxifen, induces in the animal’s genome, triggering DNA repair and the resulting epigenetic modifications. Importantly, these DNA breaks induced in the system—dubbed “ICE,” for Inducible Changes to the Epigenome—do not lead to changes in DNA mutation rates, thus ruling out the possibility that any observed consequences of ICE stem from mutations.
This is a neat and “elegant system to induce epigenetic aging, that is, to create DSBs in cells and mice without causing mutations,” writes Chinese Academy of Sciences aging researcher Guang-Hui Liu in an email to The Scientist. “I think the authors used a clever method to solve this problem,” he adds.
According to the study, there were no observable differences between mice with the transgenic endonuclease and controls at 4–6 months of age after both groups were treated with tamoxifen for three weeks. However, ten months after the treatment, “we found a lot of aging phenotypes,” such as gray hair, muscle weakness, and memory loss, says coauthor and Harvard Medical School geneticist Jae-Hyun Yang, adding that the ICE animals’ aging appeared to be an accelerated form of normal aging, as they resembled older wild-type mice. When the team looked at the epigenetic clocks, they also found that aging progressed around 50 percent faster in ICE mice than in controls.
By using ChIP-sequencing, a method that reports protein interactions with DNA, the team observed that DNA breaks and subsequent repair lead to the erosion of the epigenetic landscape. This means that while, normally, cells have genomic regions with high levels of histones bound to them and other regions with fewer of these proteins, Yang explains, DNA damage repair reduces this strong variation throughout the cells’ DNA, leading to a smoother epigenetic landscape. This, in a way, blurs the cell’s identity, which in turn means losing function, says Yang.
Finally, the team tested whether they could reset the epigenomic landscape in these ICE mice. For this, they induced the expression of a subset of Yamanaka factors, genes that can reprogram adult cells into a pluripotent state, which have been previously shown by Sinclair’s team and others to extend mouse lifespan and cure blindness. After five weeks of continuous expression of these genes in ICE mice, the team found significant signs of rejuvenation at both the molecular and tissue level.
See “Cell Re-Programmers Take the Nobel”
These results, together with those from a 2020 study in which Sinclair’s team restored vision in mice, suggest that there is a “backup copy of the software that we could reinstall into cells,” Sinclair says. That is to say, expression of the Yamanaka genes can somehow trigger cells to access data stored within that resets the epigenetic landscape. “But how that actually works, and where the information is stored, we don’t know yet,” he says, adding “that’s, for us, the next big question to answer.”
The concept of a backup copy “makes sense, simply because epigenetic information is reset every time a new baby is conceived,” the University of Rochester’s Vera Gorbunova writes in an email to The Scientist. “Most likely the information is encoded in the DNA, but the restoration program is only activated under specific circumstances (such as in the developing embryo),” adds Gorbunova, who did not participate in this study but peer-reviewed it.
Gorbunova says that these findings can potentially be translated into a treatment to restore epigenetic information in human cells and tissues, but “we just have to find a very safe way of doing it.” Sinclair, who is a consultant and board member of several biotechnology companies, says his team is currently working on such a therapy: In 2017, with this goal in mind, he started the Boston-based company Life Biosciences. He says “there’s been a lot of effort [and] tens of millions of dollars spent on this already.” He adds that the company is currently focused on “nonhuman primate studies for improving vision,” and those results will come out in the next few months. “If that works, the next species is human.”
If the team succeeds in safely manipulating epigenetic landscapes in humans, he continues, “what we currently think of as very different diseases,” such as Alzheimer’s, diabetes, cancer, and heart disease, could be treated “all with one medicine, and that’s what we’re aiming for.”
He claims that “these diseases go away” if a treatment manages to make “the body younger . . . because they’re all manifestations of aging,” and that’s what he says is “the big deal of finding a universal cause of aging.”