ABOVE: Joseph Kreitz, MIT
Sophisticated, effective drugs to treat diseases and other conditions aren’t any good if they can’t reach the part of the body or the specific cells that they’re designed to target. However, scientists have found a new way to deliver tiny proteins into specific cells, using small syringelike structures naturally found on certain bacteria. The study, published in Nature on March 29, could lead to better drug-delivery systems in medicine.
“Delivery remains a critical bottleneck in medicine,” said study coauthor and MIT researcher Joseph Kreitz. “Although many powerful new therapies have been developed over the past several decades, we will need a deep bench of options to get these therapies into the right cells in the body.”
In the study, Kreitz, Broad Institute researcher Feng Zhang, and the rest of their team took inspiration from nature, relying on tiny microbes that have found a way around this problem. Endosymbiotic bacteria, or bacteria that depend on their host cells for survival, have developed tools such as the extracellular contractile injection system (eCIS), in which the bacteria use tiny syringelike nanomachines to inject protein payloads into their host cells. The host cells, in the case of the bacterium Photorhabdus asymbiotica, are the cells lining the gut of nematodes. In the new study, Zhang and the team re-engineered these so-called nanosyringes from Photorhabdus to target and deliver a wide variety of proteins into human and animal cells.
See “Drugs Hitch a Ride on Algae for Targeted Delivery”
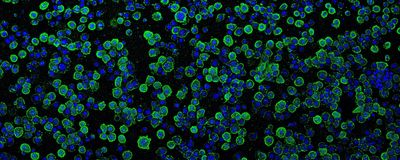
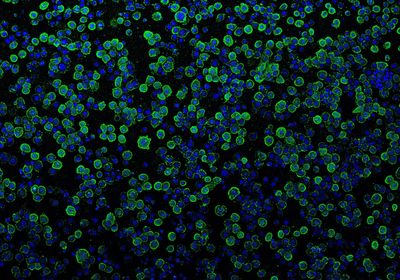
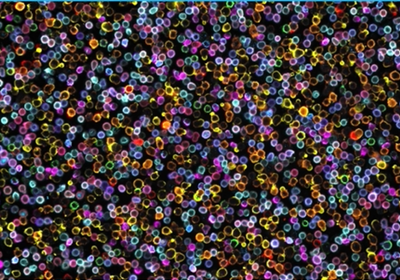
The researchers first confirmed that the Photorhabdus virulence cassettes (PVCs) could deliver nonnative proteins in host cells. They used the Cre-loxP system for these experiments, wherein GFP expression in the host cells was prevented by a STOP codon, flanked by the loxP sequence. On adding Cre recombinase, the enzyme recognized the loxP sites and excised the STOP codon. Thus, active GFP expression served as an indicator of successful Cre delivery into the cells.
But the true challenge lay ahead: to use PVCs to target human or mouse cells—cells very different from the insect host cells the PVCs were known to target. This was compounded by the fact that scientists weren’t even sure how PVCs recognize insect cells in the first place. What was known though, is that these PVCs resemble structures used by bacteriophages, viruses that use contractile tails to inject their genetic material into bacteria.
“We suspected that the PVCs recognized cells via small protein filaments called tail fibers, but it was not initially clear how we would need to modify these tail fibers to alter the target specificity of this system,” Kreitz said.
Using AlphaFold, the powerful AI platform that can predict the 3D structure of a protein from its amino acid sequence, the team could model the PVC’s tail fiber to better understand how it binds to its target receptor. The researchers then re-engineered the PVC tail fibers to specifically recognize a receptor on human lung adenocarcinoma cells. Using the re-engineered tail fibers, they were able to load different kinds of proteins into these cells in vitro: the bacteria’s native toxic proteins, which killed the cells, and nonnative Cre, which turned the cells green. They now had a delivery tool which could—specifically and effectively—microinject proteins into human cells.
“I can imagine the programmable nature of this approach may be useful in achieving improvements in target or tissue selectivity in the future,” Angela Koehler, a researcher at MIT who was not involved in this study, told The Scientist.
See “Now AI Can Be Used to Design New Proteins”
Next, the researchers tested the system’s ability to deliver CRISPR genome editing components to target cells in vitro. While CRISPR technology has been widely adopted for therapeutic research, targeted delivery remains a major challenge in the field. “We keep expanding this tool box of delivery modalities; we have a tool box of genome editing machines, types of molecules to deliver, and now we are expanding the delivery toolbox itself,” Rodolphe Barrangou, a researcher working with CRISPR at North Carolina State University who was not involved in this study, told The Scientist.
The team was able to inject Cas9 protein, a nuclease involved in CRISPR-mediated gene editing, into human cells expressing a guide RNA, to effectively edit the genome in those human cells. The PVCs with modified tail fibers were very specific to their target receptors, a key feature that can be exploited in its future applications as a potential therapy against cancer cells.
See “Bacteria as Living Microrobots to Fight Cancer”
“We are excited by the possibilities these systems provide for future applications,” said Kreitz. “For example, because PVCs can deliver proteins, in contrast to DNA- or RNA-based delivery systems which deliver blueprints for proteins, they might provide us better control over the dose and half-life of a therapeutic inside cells.”
As a final test of the new system’s efficacy, Kreitz and his colleagues used the PVCs to inject proteins safely and successfully into a live mouse’s brain, after modifying the tail fiber to recognize receptors on a mouse cell. They again used the Cre-Lox system and confirmed that PVC-delivered nonnative proteins perform their function correctly in vivo. Also, the injection did not lead to any significant immune response and the PVCs did not stick around in the mouse brain for longer than a week after the injection—adding to the list of features that support the use of this tool as a potential therapeutic in the future.
And the researchers are already involved in potentially commercializing this technology. According to the paper, Kreitz and Zhang are listed as coinventors on a US provisional patent application filed by the Broad Institute entitled “Cell-Type Specific Targeting Contractile Injection System.” Zhang is a scientific advisor and cofounder of Editas Medicine, Beam Therapeutics, Pairwise Plants, Arbor Biotechnologies, and Aera Therapeutics. Zhang is also a scientific advisor for Octant.
“We are interested in further understanding its immunogenic properties, tissue penetration, and organ localization,” said Kreitz. “Eventual use of PVCs in human therapeutics will require further preclinical development and rigorous, FDA-regulated, clinical studies to ensure this system is safe and efficacious.”
“It is a great proof of concept,” Barrangou said. “Illustrating the potential of this technology with genome editing, in vivo in neurons, there are reasons to be excited. It is an area of future interest, an area of great therapeutic potential, and an area of great technical difficulty.”
It may be possible to use these PVCs as a drug-delivery tool to treat human disease in the future. At present, they are a programmable protein-delivery tool that can be modified to target a whole variety of cells from different organisms, ranging from insects to humans.
“It’s very hard to deliver payloads to neurons and brain tissue, and being able to do that, I think, is a very encouraging start, albeit being in the early stages,” said Barrangou.