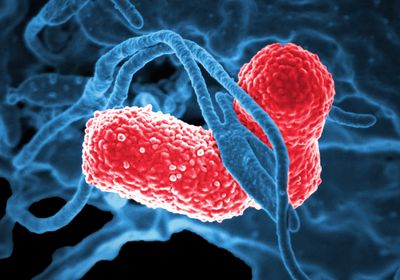
ABOVE: Scanning electron micrograph of Klebsiella pneumoniae, a related bacterium often implicated in hospital-acquired infections David Dorward, PhD; National Institute of Allergy and Infectious Diseases (NIAID)
Klebsiella aerogenes, a bacterium associated with poor clinical outcomes in hospitals, is more prevalent in the gut of premenopausal women with depression than in premenopausal women without it, reports a study published today (March 17) in Cell Metabolism. The authors identified a key enzyme in the bacterium’s genome that degrades the ovarian hormone estradiol. Mice fed this bacterium or a different one engineered to carry the enzyme had lower estradiol levels and evidence of depressive-like behaviors compared to control mice.
Declining estradiol levels have been linked to female depression in humans. After finding that the levels of this steroid hormone were significantly lower in 91 menopausal women with depression than in 98 menopausal women without this mood disorder, a team at the Renmin Hospital of Wuhan University, China, explored the influence of the gut microbiome on these differences. By incubating the fecal microbes of samples from either of both groups with estradiol, the team found that those from patients with depression were significantly more efficient at degrading estradiol than those from the nondepressive group. Furthermore, fecal transplants from samples from the depressed group to mice induced depression-like behaviors in the animals.
In search of the species responsible for this degradative activity, the researchers cultured the fecal samples from the group with depression on a medium in which the only carbon source was estradiol. Under these conditions, “a pale white colony with fuzzy edges and a smooth surface” grew, the researchers write in their paper, which they identified as a strain of the Gram-negative K. aerogenes. By sequencing its genome, the team further found the presence of an estradiol-degrading enzyme—an enzyme that, in earlier work, a team led by the same researchers had reported also degrades testosterone, inducing depressive-like behaviors in male mice.
Engineering this enzyme into an Escherichia coli strain and feeding it to female mice was sufficient to reduce the animals’ blood, lower brain, and hippocampus estradiol levels and induce depressive-like behaviors. By doing this final step, the team confirmed that this enzyme is “crucial” to what they are observing and that it is the activity of this enzyme that “is causing these effects,” says Brittany Needham, a microbiologist and neuroscientist at Indiana University School of Medicine, who was not involved in this work.
Finally, analyses of both groups of premenopausal women revealed that those exhibiting depression had significantly higher abundances of K. aerogenes and its estradiol-degrading enzyme in fecal samples.
“They showed really nicely the causality in mice,” that is, that feeding mice with bacteria carrying the enzyme modified the animals’ estradiol levels and behavior, says Needham. But this has yet to be demonstrated in humans, where, so far, there is only an association.
University of North Carolina-Chapel Hill School of Medicine’s David Rubinow, who did not participate in this study, writes in an email to The Scientist that even though animal studies like this one “certainly provide indications that [alterations of] gut bacteria can have quite striking phenotypic effects, for humans, there is at this time more smoke than fire.” Yet, he adds, “these data will encourage further studies of the [role of the] microbiome in affective disorders.”