ABOVE: © ISTOCK.COM, PETERSCHREIBER.MEDIA
We have been at war with viruses for more than a billion years. This intensifying arms race has fine-tuned our immune systems and yielded new heights of viral trickery. Some DNA viruses are known to alter chromatin folding, suppressing immune genes such that they can infect cells more readily. But it was long unclear whether RNA viruses, including SARS-CoV-2, perform a similar stunt, Wenbo Li, a biochemist at the University of Texas’ Health Science Center, tells The Scientist.
Now, in a study published March 23 in Nature Microbiology, Li and colleagues reveal how the virus responsible for COVID-19 remodels chromatin, the complex of DNA and proteins that makes up chromosomes. The resulting changes in gene expression may be responsible for the immune dysregulation seen in infected people and may offer clues as to why some experience prolonged symptoms.
Viruses don’t just trigger a brief spell of sickness, says Marianna Zazhytska, a biophysicist at Columbia University, who was not involved in the work. “These pathogens, especially viruses, are interacting with our genome which can have long-lasting consequences,” she adds.
See “SARS-CoV-2 Infection Can Alter Future Immune Responses”
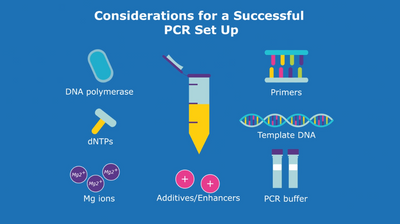
The researchers behind the new paper infected cultured human lung cells with SARS-CoV-2 and analyzed chromatin’s 3D architecture, the progressive folding into chromosomal compartments, domains, and loops. Compartments come in two flavors: A and B. The A compartment contains genes that are transcriptionally active while the B compartment houses genes that tend to be silenced. “They are like the yin and yang of chromatin,” says Li. “Due to their chemical features, they separate and do not mix,” he says. The DNA within each compartment bends and folds into domains, which brings the gene in alignment with regulatory sequences.
Cells infected with either an inactive version of SARS-CoV-2 or a different type of coronavirus contained chromatin organized in compartments with neat domains. But lung cells infected with active SARS-CoV-2 contained sections of chromatin that had lost features of their A/B identity and were intermingled with the other compartment.
Probing further, the researchers found that the muddled regions contained genes that are typically activated in response to viral infection, such as those that code for interferons. That interference with immune genes may explain the findings of a previous study that showed infected patients release just a trickle of interferons in response to SARS-CoV-2 even though they mount a robust response to other viruses. “The chromatin change provides an unappreciated mechanism to think about how the virus antagonizes our cellular defenses,” Li says.
A closer look within each chromosomal compartment revealed that some of the domains had lost their shape. In uninfected cells, a protein complex called cohesin encircles each domain, forming tight loops that bring each gene close to an activating region. But cohesin proteins are depleted in SARS-CoV-2–infected cells and the domains are too loosely folded for transcriptional activation. This is yet another way that SARS-CoV-2 may manipulate the expression of immune genes, says Li.
See “Mechanism of a Genome Packaging Machine Discovered”
But how exactly does COVID-19 remodel chromatin? One mechanism may be through epigenetic changes. The infected cells were missing an acetyl group—known as H3K27Ac—on their third histone that’s associated with transcriptional activation. Removal of this group is likely to suppress neighboring genes. H3K27Ac depletion correlated with regions that lose their A/B identity, the study found, suggesting that the marker’s absence may underlie the structural changes, says Li. In fact, another recent study found that SARS-CoV-2 uses the host cell’s machinery to synthesize a protein that thwarts acetylation by mimicking the host’s histones.
“Histone modifications are known to have long-term residual timing,” says Li. The alteration can persist, particularly in lung cells which have a longer lifespan than many other kinds of cells, he adds. Therefore, these epigenetic changes could be the molecular basis of long COVID, and further work could pave the way for therapeutic interventions, he says.
Scientists are now beginning to understand the mechanisms underlying brain fog and other long-term symptoms of long COVID, says Zazhytska. But more work is needed to reveal whether the same changes that are detected in a single cell line also occur within a whole organism, where multiple cell types are interacting, she says.
See “Multiple Possible Causes of Long COVID Come into Focus”
Juan Fuxman Bass, a Boston University systems biologist who was not involved in the study, argued a similar point. He notes that some signs of long COVID, such as altered T cell activity, may have nothing to do with changes in the chromatin landscape. “Long COVID is a very complex disease that involves many different cell types, some of which are not even infected with SARS-CoV-2,” he says.