Parkinson’s disease is the second most common neurodegenerative disorder, affecting more than ten million people worldwide. The breakdown of dopaminergic neurons in a brain region involved in movement, called the substantia nigra pars compacta, causes Parkinson’s disease symptoms, including tremors, impaired movement and stiffness, and disrupted balance. As the incidence of Parkinson’s disease continues to increase, this disorder places a large burden on patients, caregivers, and the healthcare system, so therapeutics that treat its pathology are urgently needed.1,2
While most cases are sporadic or idiopathic with no known specific cause, Parkinson’s disease can be familial, caused by inheriting a mutated gene, such as leucine-rich repeat kinase 2 (LRRK2). Scientists are testing LRRK2-specific kinase inhibitors to treat Parkinson’s disease, and an LRRK2-targeted drug recently advanced into phase III clinical trials.1,3 In a Nature Structural and Molecular Biology paper, Samara Reck-Peterson, an investigator and professor at Howard Hughes Medical Institute, in collaboration with Andres Leschziner at University of California, San Diego, highlights the complexity of targeting LRRK2 for Parkinson’s disease treatment.3
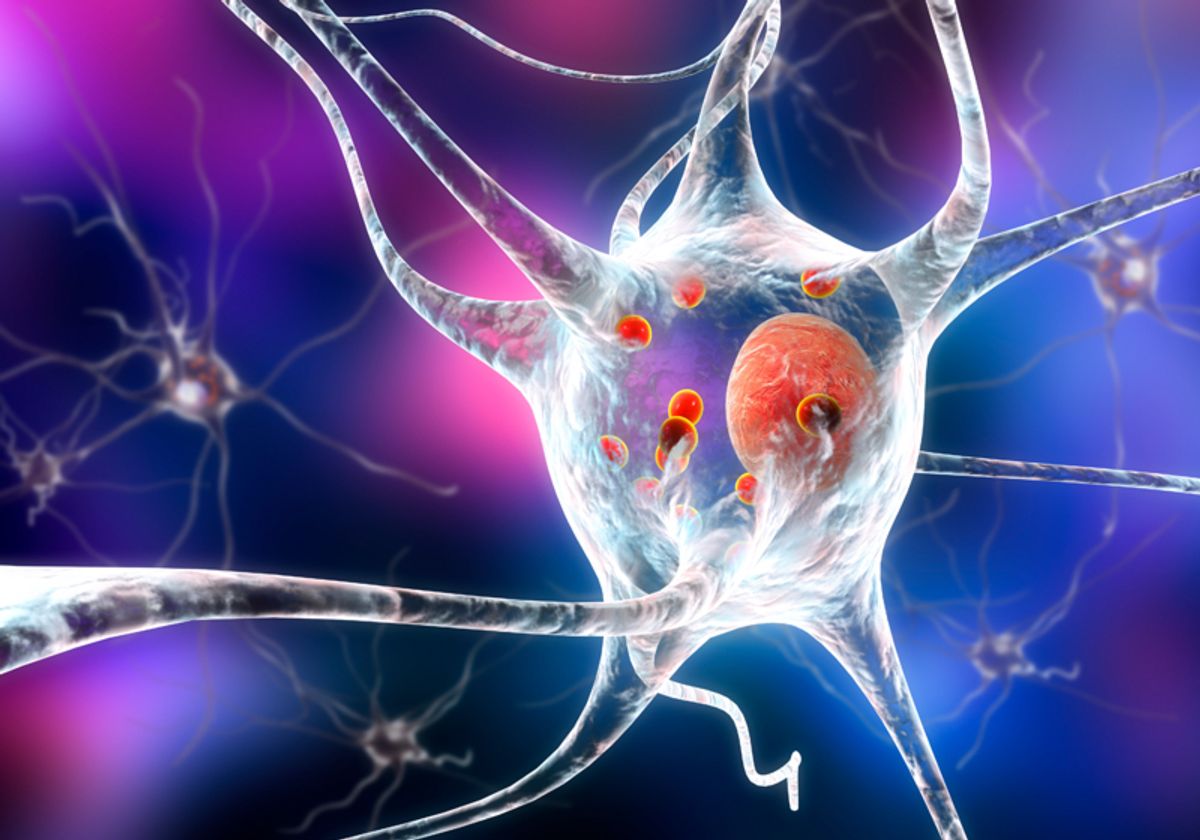
Several researchers previously analyzed the structure of LRRK2 and found that this protein can interact with microtubules.3-5 Using cryo-electron microscopy (cryo-EM), Reck-Peterson’s team identified the specific LRRK2 amino acids that mediate this interaction. Mutating these amino acids disrupted microtubule binding in a test tube and in cell culture. The researchers also confirmed that LRRK2 is in a closed, active conformation when it binds to microtubules, which has implications for choosing the right kinase inhibitor when treating familial Parkinson’s disease.
Two types of kinase inhibitors target LRRK2, both of which use different mechanisms to turn off kinase function. Type 1 LRRK2-specific kinase inhibitors stabilize the protein’s closed conformation, while the type 2 group are non-specific kinase inhibitors that force LRRK2 into an open conformation. Stabilizing LRRK2 in either conformation will prevent its kinase activity.
If we put those two [together], the clinical similarity, and then this overlapping mechanism, it actually suggests this is a pretty good target for most kinds of Parkinson's disease.
- Mark Cookson, National Institute on Aging
Researchers are testing type 1 inhibitors in clinical trials because they are more specific and more potent than type 2 inhibitors.3,4 However, Reck-Peterson’s structural analysis confirms previous findings that some type 1 inhibitors increase LRRK2’s microtubule binding.5 This is concerning because LRRK2 can act as a roadblock for molecular motors that move along the microtubules, impeding intracellular trafficking. “Stopping traffic in a cell is a bad thing…[It] would be something you would want to tightly control,” said Reck-Peterson. Her collaboration with Leschziner aims to determine if LRRK2 kinase inhibitors actually disrupt this trafficking.
Understanding the structure of LRRK2 has important implications for familial Parkinson’s disease drug design, and has been an ongoing, complex process for researchers in the field. “This latest paper, I think, really clarifies and adds to some of that picture that's developed,” said Mark Cookson, a senior investigator and chief of the National Institute on Aging, who was not involved in the study. In addition to informing familial Parkinson’s disease therapeutics, this added clarity to the LRRK2 picture may lend insight to overlapping mechanisms between familial and sporadic Parkinson’s disease linked to LRRK2 mutations.
“The familial cases that are driven by LRRK2 mutations, their clinical phenotype, their progression, and their range of symptoms are all…very similar to idiopathic Parkinson's disease,” explained Cookson. “LRRK2 is also what we call a genetic risk factor for otherwise sporadic PD [Parkinson’s disease]…So if we put those two [together], the clinical similarity, and then this overlapping mechanism, it actually suggests this is a pretty good target for most kinds of Parkinson's disease.”
References
- A. Oun et al. “Characterization of lipopolysaccharide effects on LRRK2 signaling in RAW macrophages,” Int J Mol Sci, 24(2):1644, 2023.
- P. Martinez-Martin et al. “Impact of advanced Parkinson’s disease on caregivers: an international real-world study,” J Neurol, online ahead of print, 10.1007/s00415-022-11546-5:1-12, 2023.
- D.M. Snead et al., “Structural basis for Parkinson’s disease-linked LRRK2’s binding to microtubules,” Nat Struct Mol Biol, 29(12):1196-1207, 2022.
- A. Tasegian et al., “Impact of type II LRRK2 inhibitors on signaling and mitophagy,” Biochem J, 478(19):3555-73, 2021.
- A.E. Leschziner, S.L. Reck-Peterson, “Structural biology of LRRK2 and its interaction with microtubules,” Mov Disord, 36(11):2494-2504, 2021.